ECOSHELTA has long been part of the sustainable building revolution and makes high quality architect designed, environmentally minimal impact, prefabricated, modular buildings, using latest technologies. Our state of the art building system has been used for cabins, houses, studios, eco-tourism accommodation and villages. We make beautiful spaces, the applications are endless, the potential exciting.
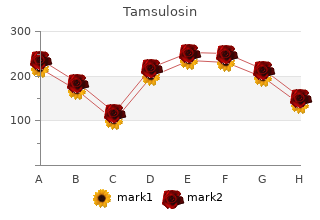
2018, Lincoln University, Jefferson City Missouri, Jose's review: "Tamsulosin 0.4 mg, 0.2 mg. Discount Tamsulosin no RX.".
The use of corticosteroids to treat renal failure associated with AIN remains controversial buy tamsulosin 0.2mg online androgen hormone x for hair. No randomized buy generic tamsulosin 0.2 mg on-line mens health nutrition manual, controlled trials have yet proved that corticosteroid therapy has any advantages over discontinuance of medication. A 65-year-old man with hypertension and reflux disease presents to your office for routine follow-up. Laboratory data reveal an increased serum potassium level of 5. On ques- tioning, you learn that the patient has a history of hesitancy, dribbling, and a decrease in the urinary stream. Which of the following statements pertaining to renal interstitial damage from physical factors is false? For patients with vesicoureteral reflux, medical therapy is unhelp- ful, and surgical intervention should be recommended immediately B. In patients older than 60 years, the most common causes of obstruc- tive uropathy are benign prostatic hypertrophy and prostatic or gynecologic malignancies C. Ultrasonography is the diagnostic test of choice for obstructive nephropathy D. Before diagnosing a patient as having vesicoureteral reflux disease, any urinary tract infection should be treated if present, and a repeat voiding cystourethrogram should be performed Key Concept/Objective: To know that vesicoureteral reflux can cause chronic tubulointerstitial damage, known as reflux nephropathy Vesicoureteral reflux can cause chronic tubulointerstitial damage, known as reflux nephropathy. When infection is present, even low-pressure refluxed urine that reaches the kidney can produce chronic interstitial inflammation and scarring. Presenting fea- tures can include such signs of urinary tract infection as back or flank pain, fever, and dysuria. Hypertension, when present, is often associated with high levels of renin, which may derive from the segmental areas of scarred parenchyma. Patients often have a urinary concentrating defect, leading to nocturia and polyuria. Reflux is demonstrat- ed with a voiding cystourethrogram. Because urinary tract infection may be associated 10 NEPHROLOGY 23 with reflux, it is best to wait several weeks after treating a urinary tract infection before trying to diagnose reflux nephropathy. Treatment of low-grade reflux is medical: long- term antibiotic therapy is used to sterilize the urine and prevent reinfection. Many per- sons with mild reflux undergo spontaneous remission with time. More severe reflux may require surgical intervention, although most comparative studies have not found an advantage for surgical intervention over medical therapy. Obstructive nephropathy may produce chronic interstitial damage, especially when the obstruction is partial or intermittent and longstanding. In persons older than 60 years, benign prostatic hyper- trophy and prostatic and gynecologic cancers are common etiologies. The pathologic findings show dilatation of the collecting ducts and distal tubules. Ultrasonography usually shows dilatation of the urinary collecting system and hydronephrosis. A 38-year-old man comes to your office for evaluation of a urinalysis that revealed proteinuria. Further evaluation demonstrated proteinuria in the nonnephrotic range and a creatinine level of 1. The patient has celiac disease with steatorrhea, which was diagnosed many years ago. You suspect he has chronic interstitial nephritis that is associated with celiac disease. Which of the following scenarios is NOT associated with tubulointerstitial nephritis? A patient who several years ago underwent stomach bypass surgery for morbid obesity B.
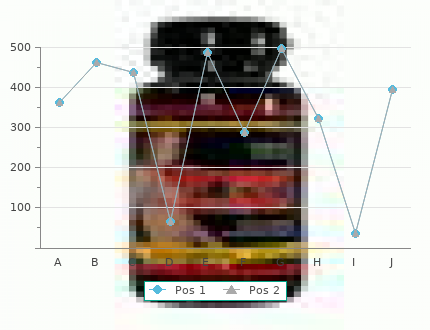
There is a deficiency of amylo-1 0.4 mg tamsulosin prostate 5 2,6-glucosidase (AGL) that catalyzes both a transferase and a hydrolysis reaction discount tamsulosin 0.2 mg free shipping mens health 4 positions. In GSD V several mis- sense, stop, start codon or frameshift mutations of 11q13 have been described. There is a deficiency of muscle phosphorylase resulting in impaired ATP generation from aerobic and anaerobic glycolysis and reduced production of pyruvate. GSD VII is due to a deficiency of 6-Phosphofructokinase (PFK – 1cen- q32). Other listed enzyme deficiencies resulting in defects of glycogen storage include: GSD XII – Aldolase A: 16q22, GSD XIII – β-Enolase: 17pter, GSD XI- Lactate dehydrogenase: 11p15, GSD IX – Phosphoglycerate Kinase: Xq13, X – Phosphoglycerate Mutase: 7p12, and GSD VIII – Phosphorylase β kinase: Xq12. Laboratory: Diagnosis The serum CK is usually very high. The ischemic forearm test shows an insufficient rise in venous lactate, but is non-specific for the GSD, relies on patient compliance, and may have complications such as myoglobinuria. Other changes include hyperuricemia, hyperbilirubinemia, and a high potassium with exercise. GSD VII is associated with a compensated hemolytic anemia. Electrophysiology: Nerve conduction studies are usually normal, however in GSD III there is often evidence of an axonal neuropathy. During contractures, the muscle is electri- cally silent in GSD. EMG shows an increase in insertional activity in distal muscles, along with short duration motor unit action potentials typical of myopathy. Myotonic discharges may be observed, and in GSD II there may be a mixture of myotonic and complex repetitive discharges observed especially in paraspinal muscles. In GSD VII repetitive nerve stimulation at 20 Hz results in a decrement in the motor response. Electron microscopy shows glycogen in cytoplasm with membrane- bound, autophagic vacuoles. In GSD III, V, and VII there are subsarcolemmal and intermyofibrillar vacuoles (Fig. In GSD VII, partial reductions in PFK to 20% of normal may be artifactual due to the lability of the enzyme in incorrect- ly handled fresh frozen muscle. Genetic testing: Genetic testing is not currently clinically available for most of these disorders. Differential diagnosis – Other glycogen storage diseases – Other metabolic myopathies – Mt myopathies – Congenital myopathies Therapy Hypoglycemia in children needs to be treated with frequent feeding. A high protein diet may improve weakness in adult forms of GSD. In GSD VII patients should avoid high-carbohydrate meals that exacerbate the “out-of-wind” phe- nomenon, and a ketogenic diet may help. Other potential treatments for GSD V are pyridoxine therapy that improves symptoms in some patients and creatine monohydrate that improves anaerobic but not aerobic exercise capability. Adenoviral-mediated delivery of a myophosphorylase cDNA into myoblasts from patients with McArdle’s disease restores myophosphorylase to normal levels, and may prove beneficial as a potential future treatment. Enzyme replacement therapy is also being evaluated in GSD II. Prognosis In GSD II (infantile form) death occurs before 1 year of age, in the childhood form before 25 years. In infantile GSD III death occurs before 4 years, child- hood and adult forms survive longer. In other forms of GSD life expectancy may be normal unless severe myoglobinur- ia and muscle necrosis occurs. References Chou JY (2001) The molecular basis of type 1 glycogen storage diseases. Curr Mol Med 1: 25–44 DiMauro S, Lamperti C (2001) Muscle glycogenoses. Muscle Nerve 24: 984–999 Martin MA, Rubio JC, Buchbinder J, et al (2001) Molecular heterogeneity of myophospho- rylase deficiency (McArdle’s disease): a genotype-phenotype correlation study.
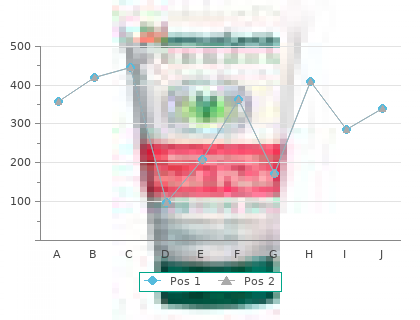
He had been both- ered only slightly by symptoms of mild urinary hesitancy and occasional frequency generic 0.4 mg tamsulosin with amex prostate oncology kalispell. Today order tamsulosin 0.2mg online prostate cancer 35 years old, however, he 10 NEPHROLOGY 35 complains that since his last visit, his symptoms of straining, hesitancy, dribbling, incomplete empty- ing, and urinary frequency have been gradually worsening. After further discussion with the patient, you decide to start treatment with terazosin. Which of the following statements regarding the use of alpha-adrenergic blockers for the treatment of lower urinary tract symptoms of BPH is true? Long-term treatment with alpha-adrenergic blockers has been shown to result in a decrease in prostate size B. Treatment with alpha-adrenergic blockers can lower the PSA level, thereby altering the cutoff value at which one would be concerned about cancer C. Alpha-adrenergic blockers induce relaxation of prostatic smooth muscle and may relieve the dynamic component of bladder outlet obstruction D. Terazosin can usually be initiated at a dose of 10 mg, given before bedtime; a majority of men will achieve notable symptom relief at this dosage E. Studies have shown that alpha-adrenergic blockers are significantly less effective than the 5α-reductase inhibitor finasteride in reducing BPH symptom scores Key Concept/Objective: To understand the important aspects of drug therapy for BPH Alpha-adrenergic blockers are among the mainstays of medical therapy for symptoms of BPH. In the absence of complications, the decision to initiate medical therapy depends in large part on the degree to which the patient is bothered by lower urinary tract symptoms. Symptom scores such as those based on the American Urology Association Symptom Index or IPSS can gauge severity of symptoms and help guide treatment decisions. Alpha-adrenergic blockers work by binding to alpha1-adrenocep- tors in the tissue of the bladder neck and reducing neuromuscular tone. They do not, however, have any impact on prostate size or PSA levels (in contrast to finasteride, which lowers PSA levels). Side effects of alpha-adrenergic blockers include orthostatic hypotension, dizziness, and asthenia. Most physicians initiate terazosin at a dose of 1 mg at bedtime for several days to avoid "first-dose" hypotension. The average effective dose of terazosin is closer to 10 mg; the dose should be gradually titrated up to this level in the absence of limiting side effects. Finasteride works by blocking the conversion of testosterone to dihydrotestosterone, which is a mitogen for prostatic tissue growth. Although this therapy may result in an actual decrease in prostate size, the average reduction in symptoms, as reflected in the IPSS, has been much more modest than that achieved with alpha-adrenergic blockers (total score reduction of 2 to 3 points for finas- teride, versus 6 to 8 points for alpha-adrenergic blockers). A 50-year-old man presents to your clinic complaining of ringing in his right ear and of feeling as if the room is spinning around him. His wife points out that he is also losing his hearing. You suspect that he is suffering from Meniere syndrome. Which of the following statements about Meniere syndrome is false? Meniere syndrome is characterized by tinnitus, vertigo, and hearing loss B. Patients suffering from Meniere syndrome can have sudden attacks, during which they fall to the ground C. Episodes of vertigo and deafness in Meniere syndrome can last for hours to a day D. The deafness associated with Meniere syndrome begins with an inabili- ty to hear low-frequency sounds and later progresses to involve higher frequency sounds Key Concept/Objective: To be familiar with the presentation of Meniere syndrome Although episodes of vertigo associated with Meniere syndrome usually last from hours to a day, deafness is constant after it develops. The deafness is characterized initially by a compromised ability to hear low-frequency sounds. Meniere syndrome is the result of excessive production and decreased absorption of inner ear endolymphatic fluid, resulting in endolymphatic hydrops. Patients usually complain of unilateral attacks of tinnitus (some have bilateral attacks), vertigo, and fullness in an ear. Tumarkin otolithic crisis is a sudden spell of falling to the ground associated with Meniere syndrome.
Use of NSAIDs and Helicobacter pylori infection are the two most important risk factors purchase tamsulosin 0.4 mg visa androgen hormone joint; heavy alcohol ingestion and smoking are also associated with PUD bleeding risk buy tamsulosin 0.2 mg on-line man health tips in hindi. A 39-year-old woman with a history of cirrhosis presents to the emergency department with massive hematemesis. Volume resuscitation with intravenous normal saline is initiated, and emergent EGD is planned for further evaluation and management. Which of the following endoscopic interventions is considered first-line therapy in the management of esophageal varices? Injection therapy Key Concept/Objective: To understand that band ligation is first-line therapy for the manage- ment of esophageal varices With variceal bleeding, endoscopic treatment is used primarily for esophageal varices; the techniques include sclerotherapy and band ligation. Sclerotherapy utilizes a variety of scle- rosants to induce variceal thrombosis, with sodium tetradecyl sulfate and ethanolamine oleate used most frequently. Complications include retrosternal chest pain, low-grade fever, ulceration (usually deep ulcers that heal within 3 weeks), dysphagia, delayed perfo- ration (1 to 4 weeks later), and stricture formation. The popularity of sclerotherapy has diminished as a result of these complications. Intravariceal injections are more effective than paraesophageal injections in controlling bleeding. Band ligation is now considered the first-line endoscopic therapy for esophageal varices. The band ligator is readily attached to the distal end of the endoscope, which is advanced to the varix; the endoscopist then suctions the varix into the ligator cap and deploys a rubber band around the varix. This results in the plication of the varices and sur- rounding submucosal tissue, with fibrosis and eventual obliteration of varices. Comparative studies report better initial control of bleeding (91% versus 77%) and rebleed- ing rates (24% versus 47%) with band ligation than with sclerotherapy. Complications of banding include retrosternal chest pain, dysphagia from compromise of the esophageal lumen, band ulceration (usually superficial ulcers that heal within 2 weeks), overtube 4 GASTROENTEROLOGY 17 injury, and perforation. A 36-year-old man presents to your clinic complaining of fatigue. Review of systems is positive for occasional diarrhea, which the patient has been experiencing for several months, and for a 20-lb weight loss. Laboratory tests reveal iron deficiency anemia, and the patient tests positive on a qualitative fecal fat test. Results of an upper endoscopy and a colonoscopy are normal. Which of the following tests would be most likely to provide helpful information in the workup of this patient? Selenium-75–labeled homocholic acid-taurine (75SeHCAT) absorption test B. Tissue transglutaminase antibody Key Concept/Objective: To understand that gluten-sensitive enteropathy (GSE) is a cause of iron deficiency anemia Patients with GSE may present with a variety of complaints, including weight loss, fatigue, abdominal cramps, distention, bloating, and diarrhea. Other presentations include iron deficiency anemia, osteoporosis, and easy bruising. In a patient in whom the suspicion of GSE is high, a positive tissue transglutaminase antibody test makes the diagnosis almost certain. Alternatively, the diagnosis might rest on small bowel biopsy findings. Another helpful test is the identification of an endomysial antibody. The presence of fecal fat is helpful in this patient because it confirms the suspicion of an underlying malabsorptive disorder. The xylose absorption test evaluates the absorptive surface area of the small bowel. The bentiromide test is a noninvasive test to evaluate for pancreatic exocrine insuf- ficiency. All of these tests can, however, be helpful in the evaluation of a patient with mal- absorption and diarrhea. On the basis of this patient’s clinical presentation, the tissue transglutaminase antibody test is the one most likely to be helpful with the diagnosis.